
David Cavern, a recovery coach who is part of an addiction specialized group at Salem Hospital, north of Boston, stands outside theemergency department
Jesse Costa/WBUR.
conceal caption
toggle caption
Jesse Costa/WBUR.

David Cavern, a recovery coach who is part of an addiction specialized group at Salem Hospital, north of Boston, stands outside the emergency department.
Jesse Costa/WBUR.
Marie lives in the seaside town of Swampscott, in Massachusetts. Last December, she started having more and more problem breathing. One early morning, 3 days after Christmas, she got up gasping for air. A voice in her head stated, “You’re going to pass away.” Marie called 911.
” I was so terrified,” Marie stated later on. Explaining that day, the 63-year-old’s voice filled with stress, and her hand clutched at her chest.
Marie was confessed to Salem Hospital, north of Boston. The staff treated her COPD, a persistent lung condition that consists of emphysema and persistent bronchitis.
After her worst symptoms decreased, a physician came the next day to check on her. He informed Marie her oxygen levels looked excellent and that she was steady and all set to be released.
NPR is not utilizing Marie’s surname due to the fact that she, like 1 in 9 hospitalized patients, has a historyof addiction to drugs or alcohol Revealing a diagnosis like that can make it tough to discover real estate, a task and even medical care in hospitals where patients with an addiction might be avoided.
However talking to the medical professional that early morning, Marie felt she didn’t have an option. She had to inform him about her other medical issue.
” He stated I might be launched,” Marie remembered. “And I stated, ‘I got to inform you something. I’m a heroin addict. And I’m, like, beginning to be in heavywithdrawal I can’t actually move, please do not make me go.'”
Without care, released patients threat overdose
At lots of hospitals in Massachusetts and throughout the nation, Marie would likely have actually been released anyhow, while still in thepain of withdrawal Maybe she would leave with a list of regional detox programs where she may– or may not– discoverhelp
However an important chance to step in and reward at the hospital would have been lost– partially due to the fact that many hospitals do not have professionals offered who understand how to reward addiction, and other clinicians do not understand what to do.
Hospitals generally use all sorts of professionals who focus on crucial organs like hearts, lungs and kidneys– or who deal with systemic or persistent diseases of the immune system or the brain. There are professionals for kids, for mental illness, for giving birth and hospice.
However if your illness is an addiction or a condition associated to drug or alcohol use, there are couple of hospitals where patients can see a clinician– whether that be an M.D., nurse, therapist or social employee– who specializesin addiction medicine
Their lack amongst hospital workers is especially striking at a time when overdose deaths in the U.S. have reached record highs, and research study programs patients face an increased threat of fatal overdose in the days or weeks after they are released from a hospital.
” They’re left on their own to figure it out, which regrettably typically indicates resuming [drug] use since that’s the only method to feel much better,” states Liz Tadie, a nurse professional accredited in addiction care.
In the fall of 2020, Tadie introduced a brand-new approach at Salem Hospital, utilizing $320,000 from a federal grant that the hospital had actually worked for a number of years to safe and secure. Tadie created what’s referred to as an “addiction seek advice from service.”
At Salem, that group consisted of Tadie, a patient case supervisor, and 3 recovery coaches– who draw on their experience with addiction to supporter for patients and help them browse their treatment options.
What an addiction seek advice from service brings to the bedside
So on that day, when Marie stated, “Please do not make me go,” her medical professional didn’t inform Marie she had to leave. He called Tadie for a bedside seek advice from.
Tadie began the treatment by very first recommending methadone, a medication to rewardopioid addiction Although lots of patients succeed on that drug, it didn’t help Marie, so Tadie changed her to buprenorphine, with much better outcomes. After a couple of more days, Marie was ultimately released and continued taking buprenorphine to handle her addiction to opioids.
However Marie continued seeing Tadie for treatment as an outpatient and was able to turn to her for assistance and peace of mind:
” Like, that I wasn’t going to be left alone,” Marie stated. “That I wasn’t going to have to call a dealership ever once again, that I might erase the number. I desire to return to my life. I simply feel grateful.”
Amongst Salem’s clinical staff, Tadie assisted get the word out about the knowledge she can use and how it canhelp patients Success stories like Marie’s assisted her make the case for addiction medicine– which likewise implied unraveling years of false information, discrimination and lack of knowledge about patients with an addiction and their treatment options.
Part of the issue, according to Tadie, is that physicians, nurses and other clinicians get really little training in the physiology of addiction and withdrawal, the medications and treatment options, and the emerging science about what works for thesepatients What little training that physicians and nurses do get is frequently unhelpful.
” A lot of the truths are dated,” Tadie states. “And people are training to use stigmatizing language– words like ‘addict’ and substance ‘abuse'”
Tadie carefully remedied physicians at Salem Hospital, for example, who believed they weren’t ever permitted to start patients on methadone in the hospital.
” In some cases I would suggest a dosage and someone would offer pushback,” Tadie states. However “we got to understand the hospital physicians and they, in time, resembled, “OK, we can trust you. We’ll follow your suggestions.”
Gradually, addiction professionals help alter the culture
Other members of Tadie’s group have actually likewise battled with discovering their location in the hospital hierarchy. David Cavern, one of the recovery coaches at Salem Hospital, is frequently the very first individual to speak to a patient who comes to the emergency spacein withdrawal He attempts to help physicians and nurses comprehend what the individual is going through and help browse their care.
” I’m most likely punching above my weight whenever I attempt to talk to a clinician or medical professional,” states Cavern. “They do not see letters after my name. It can be kind of difficult.”
However identifying addiction as a specialized, and hiring people with training in this specific illness, is moving the culture of Salem Hospital, according to Jean Monahan-Doherty, a social employee who has actually referred patients to Tadie.
” There was lastly some acknowledgment throughout the whole organization that this was a complex medical illness that required the attention of an expert,” Monahan-Doherty states. “People are passing away. This is a terminal illness unless it’s dealt with.”
Previous director of substance use disorder services at Salem Hospital Liz Tadie (left) and social employee Jean Monahan-Doherty. Tadie is moving to a brand-new task at another hospital, however Salem Hospital leaders state they are dedicated to continuing theprogram
Jesse Costa/WBUR.
conceal caption
toggle caption
Jesse Costa/WBUR.
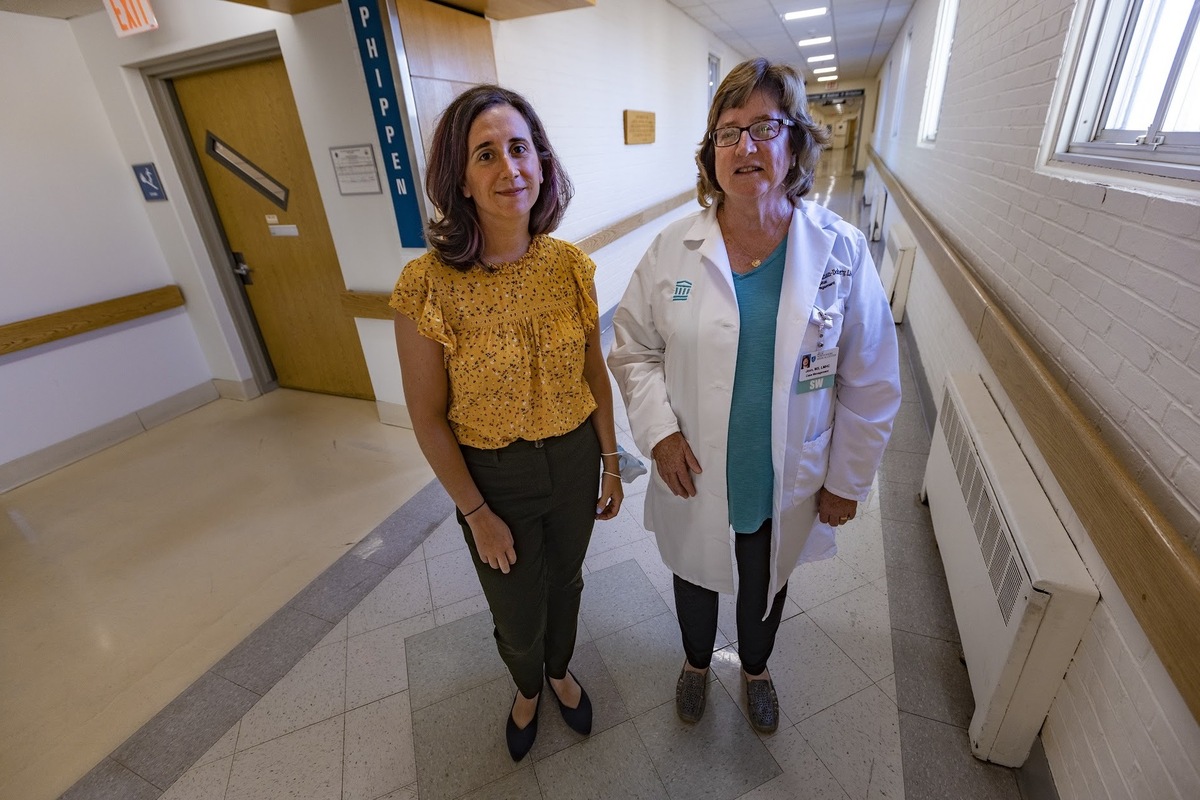
Previous director of substance use disorder services at Salem Hospital Liz Tadie (left) and social employee Jean Monahan-Doherty. Tadie is moving to a brand-new task at another hospital, however Salem Hospital leaders state they are dedicated to continuing the program.
Jesse Costa/WBUR.
This approach to treating addiction is winning over some Salem Hospital workers– however not all.
” Some of the medical staff continue to see it as an ethical concern,” Monahan-Doherty states. “In some cases you hear an mindset of ‘Why are you putting all this effort into this patient? They’re not going to improve.’ Well, how do we understand? If a patient comes in with diabetes, we do not state, ‘OK, they have actually been taught as soon as and it didn’t work. So we’re not going to use them support once again.'”
In spite of sticking around appointments amongst some associates, the need for their services is rather high. Numerous days, Tadie and her group have actually been overwhelmed with recommendations.
With federal assistance, mentions experiment to stop overdose deaths
4 other Massachusetts hospitals likewise included addiction professionals in the previous 3 years and experienced comparable obstaclesand success The extra staff were paid for by federal financing from the Recovery Communities research study This job is paying for a large range of strategies throughout a number of states, to identify the most effective methods to minimize drug overdose deaths. They consist of mobile treatment centers, street outreach teams, naloxone trainings and circulation, trips to treatment websites, and multilingual public awareness projects.
” You actually do provide much better care for patients and you make the care environment one that people are more pleased working in,” states Dr. Jeffrey Samet, who leads the Massachusetts part of this research study effort. Samet practices primary care at Boston Medical Center and states including addiction professionals in hospitals is an essential piece of the option.
Dr. Todd Kerensky, president of the Massachusetts Society of Addiction Medicine, has actually seen patients cry when they discover he specializes in addiction and desires to treat their illness, not pity them.
” It’s gut-wrenching to understand there are a lot of organizations that do not have this service,” states Kerensky. It’s unclear the number of hospitals in Massachusetts have addiction specialists on staff, however Kerensky states it’s a “unique minority.”
There are lots of possible factors. It’s a brand-new field, so discovering certified staff members with the best accreditations might be an obstacle. Some hospital leaders state they’re anxious about the costs of addiction treatment and fear they’ll lose cash on the efforts. Some physicians report not desiring to start a treatment medication while the patient is still in the hospital, due to the fact that they do not understand where to refer patients after they have actually been released, whether that be outpatient follow-up care or aresidential program To address follow-up care, Salem Hospital began what’s referred to as a “bridge center,” where patients get help transitioning to outpatient care.
In spite of these concerns and appointments, hospitals that do not have an addiction specialized group requirement to begin one, states Dr. Honora Englander, a national leader in addiction specialized programs.
” People with substance use disorder are coming to our hospitals now,” stated Englander, who directs an addiction care group at Oregon Health and Science University. “We can’t wait. We have to do much better, and this is the time.”
Englander states the federal government might support the development of more addiction seek advice from services by offering financial rewards– or charges for hospitals that do not welcome them. The Centers for Medicare & & Medicaid Providers, which has regulative authority over many U.S. hospitals, might need that hospitals stock the medications used to reward an addiction and track results for patients hospitalized with a substance use disorder, in the exact same method that CMS currently does when it comes to readmissions for other health conditions.
At Salem Hospital, the program is still brand-new, and some staff concern about its future. Liz Tadie is moving to a brand-new task at another hospital, and the federal grant ended June 30. However Salem Hospital leaders state they are dedicated to continuing the program, and the service will continue.
Compared to the other 4 Massachusetts hospitals that introduced addiction seek advice from teams utilizing the exact same federal grant, Salem Hospital has actually assisted the mostpatients Over a 15-month duration, its group assisted 448 patients start medication to treat their opioid use disorder.
This story originates from NPR’s health reporting collaboration with WBUR and KHN (Kaiser Health News).
.
